Abstract
Introduction: Extranodal NK/T cell lymphoma (ENKTL), nasal type is an uncommon, unique subset of non-Hodgkin lymphoma. Its clinical outcome has improved significantly with introduction of non-anthracycline based chemotherapy and radiotherapy. Yet little is known about central nervous system (CNS) involvement of ENKTL, nasal type.
Methods: A total of 168 patients with ENKTL-nasal type were included in this study. All patients were diagnosed between 2003.1 and 2016.6 in Asan Medical Center, Seoul, Korea. Patients with secondary CNS involvement at diagnosis and patients with aggressive NK-cell leukemia were excluded. CNS involvement was confirmed by pathology or MRI of affected organ. Cox regression analysis was performed to identify possible risk factors for CNS involvement.
Results: Out of 168 patients, 109 patients were male and 59 patients were female. Median age at diagnosis was 52 years (range: 16-83). The number of patients with stage I/II disease was 112 (66.7%) and stage III/IV was 56 (33.3%). The number of patients with low, intermediate, high prognostic index of natural killer cell lymphoma (PINK) was 70 (41.7%), 55 (32.7%), 43 (25.6%) each. Thirty (17.8%) out of 168 received anthracycline-based chemotherapy for first line treatment, either CHOP or CHOP-like regimen, and 123 patients (73.2%) had non-anthracycline based chemotherapy. Ninety two patients (54.8%) received sequential radiotherapy or concurrent chemoradiation.
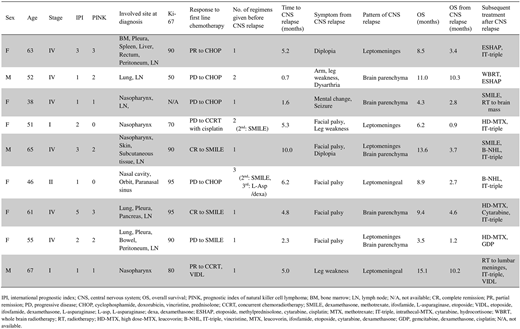
During the 63 months of median follow-up, 9 patients (5.4%) developed CNS relapse. Among those 9 patients, 4 had leptomeningeal involvement, 3 had brain parenchymal disease, and the remaining 2 had both leptomeningeal and brain parenchymal involvement.
Median time from diagnosis to CNS relapse was 5.0 months (95% confidence interval (CI): 4.6-5.3). Median OS after CNS metastasis was 3.4 months (1.6-5.1). Significant differences in OS were noted between the two groups, with median OS in patients with CNS relapse of 8.9 months (7.8-10.1) and 58 months (19.6-96.4) in patients without CNS relapse. (p<0.001)
After univariate analysis, eastern cooperative oncology group (ECOG) performance status≥2 (hazard ratio (HR) 9.7 [95% CI: 1.1-84.3] p=0.039), stage III/IV (HR 5.8 [1.5-23.5], p=0.013), lung or pleural involvement (HR 12.5 [3.3-47.5], p<0.001), peritoneal involvement (HR 46.2 [4.1-521.5], p=0.002), PINK≥2 (HR 6.2 [1.2-32.2], p=0.03) were associated with increased CNS relapse. First-line treatment regimens including etoposide or high-dose methotrexate (MTX) were associated with decreased incidence of CNS relapse. (HR 0.24 [0.06-0.88], p=0.032). Due to the small number of CNS events, multivariate analysis was not available. No association was found with age, sex, serum lactate dehydrogenase level, number of involved extranodal sites, international prognostic index, non-nasal or nasal type and Ki-67 labeling index.
Conclusions: Our study demonstrated that CNS relapse or progression in ENKTL-nasal type is rare (5.4%) but its clinical course is poor. CNS event usually occurred in the early course of the disease and we suggest that CNS evaluations should be considered in highly selected patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal